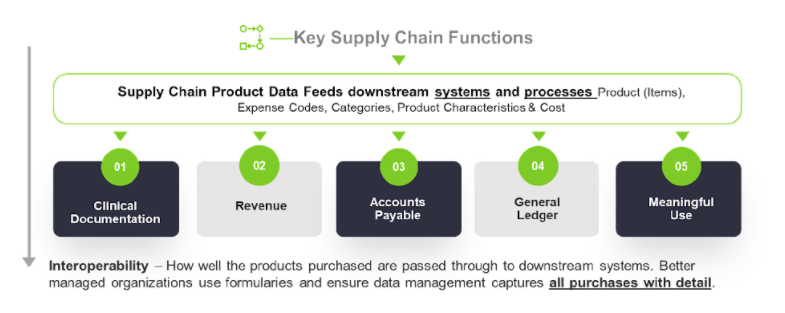
As hospital data management evolved from paper to electronic workflows into complex, integrated systems of ERP, EHR, and other connected hospital platform software, the supply chain team has always been responsible for maintaining an “item master” of all medical and non-medical products. Supply chain item masters were created and sustained to primarily support the purchase order process. But they’ve often been underfunded and overlooked on the spectrum of priorities by the supply chain team and the entire hospital.
Without a centralized source of standard product information, much of this important medical supply data has been hand-keyed or imported from Excel spreadsheets across thousands of hospitals, creating today’s challenge of aggregating this information at a macro level. In fact, an entire industry of third-party consulting, data and analytics companies evolved to help hospitals and alliances try to overcome this obstacle.
At the local level, when a hospital’s system began integrating ERP, EHR, accounting, financial and billing data, additional fields were used in the item master data to store accounting codes, UNSPSC, clinical terms, inventory flags, HCPCS and other data used throughout the cost cycle. The integrated flow of this product data with supplemental information does help users in other cost cycle functions perform their job more efficiently.
Inconsistency, Lack of Transparency and Longer Cycle Times Remain
Unfortunately, a high turnover of products, challenging data integrations, the lack of master data management (MDM) practices involving representatives outside of supply chain, no data sources to address these other areas and hand-keyed updates have resulted in inconsistency, increased cycle time and labor and lack of transparency in other cost cycle operations. Some of the issues that detract from an efficient cost cycle include:
-
General ledger codes that are missing, incorrect, or vague
-
Activity cost codes that are incorrect or inconsistent
-
Incorrect price or unit of measure issues that can delay accounts payable
-
Lack of clinical categorization to support clinical system maintenance and value analysis
-
Item master and clinical documentation systems out of sync with item adds
-
Missing item information from trunk stock items not in the system
-
Missing item description
-
Missing or incorrect HCPCS codes
-
Lack of UDI information and inability to scan/barcode at point of use
For every instance that this information is not ready to use, labor and cycle time are added to downstream departments.
You Can Close the Interoperability Gaps
You don’t have to go it alone! Consider collaborating with a partner that can fully assess your supply chain and cost cycle processes and offer technology and services to help improve your overall interoperability. Here are a few steps that will help you close some of the gaps:
-
Determine how your supply chain MDM data serves the entire cost cycle and how easily data is recognized and passed between integration points.
-
Ensure that all commonly used products have complete and consistent attributes.
-
Expand your technology to capture areas such as procedure trunk stock and consignment, including the flow of information with key attributes.
From supply chain to procedure to billing and cost accounting, when you streamline and simplify your cost cycle process, your analytics become more valuable and your operations more efficient. It’s a solution that will pay dividends for your hospital or health system in both good and bad economic times.