The cost accounting world has become enamored in the past several years with the promise of Time-Driven Activity-Based Costing (TDABC) putting an end to relative value unit (RVU) costing and its associated maintenance requirements. The entire premise of TDABC has been oversold and underdelivered, which I'll cover in a future newsletter topic.
Introduction
One area of the hospital where TDABC does not apply is in the Lab. There is no "time-stamp" data for labor, and consumable supplies account for a substantial amount of spend incurred. Many hospital labs actively seek out "outreach" business in their local communities. To sell lab services to local physician practices, nursing homes, and others, the hospital lab needs to price its testing competitively vs. the large for-profit laboratories (LabCorp or Quest). Also, Clinical Variation Reduction (CVR) efforts will look at lab testing as an opportunity for reduced utilization. For these reasons, lab managers are very interested in understanding the true costs to perform tests.
Traditional Approaches to Lab Costing
There are several methods utilized to determine RVUs for Lab tests. One simple method uses the CMS Clinical Laboratory Fee Schedule as the relative proxy for cost. CMS has studied all these tests and has set reimbursement to be consistent with cost. Or have they? There's really no transparency with this approach.
I've seen some hospitals license Lab test relative values from a third-party consulting firm. Simple, yet costly. But again, does it represent the costs actually incurred by the hospital?
The traditional default method for Lab costing is to start with the proverbial "80-20 Rule" to reduce the sheer volume of tests to look at. Then do a Bill of Materials approach on those top 80% of tests. This approach provides generally improved results for those top tests, but has a long data collection phase, maintenance can be just as time consuming, and the costs for the bottom 20% of tests can be wildly inaccurate.
An Improved Approach Using Enhanced Supply Chain Data
To properly calculate Lab test costs, one needs to understand Lab operations and the relationship to spend. I find it extremely helpful to visit a hospital Lab, talking to the clinical leaders, and getting a firsthand view of workflow. Modern hospital labs have a high degree of automation, so it is critical to understand the labor requirements, as well as the equipment-related costs (depreciation, lease, maintenance, reagent rental, etc.). Each piece of testing equipment, known by various terms such as "line", "platform", "method", "analyzer" to name a few, has its own needs for cost accounting.
The first step requires an itemization of the various platforms in use. For each platform, gather up all the relevant information:
- Manufacturer and model(s).
- Equipment-related expense (depreciation, lease, maintenance, etc.).
- Staffing coverage (hours per week) and determination of relationship to test volume.
- Export from Lab Info System (LIS) test order codes performed on each platform and test codes mapped to bill (charge) codes.
- Export from ERP containing all Lab purchase order (PO) detail for the period under study.
As you may recall from our previous newsletters and blog posts, we've made many innovations in spend normalization and categorization using a mix of proprietary and publicly available data sources. In the "good ol' days" of cost accounting, we'd ask the Lab manager to sift through volumes of data to stitch together all the relevant connections enabling RVUs to be derived. This had the potential to drag on indefinitely.
Over the past several months, we've developed an algorithm which can scan the PO history and link it to the platforms. Our proprietary categorization schemes also break down the line-item data into product types, such as:
- Reagents and kits.
- Controls and calibrators.
- Maintenance costs.
- Other misc. costs.
The entire PO history is presented in a grid format with tools to allow sorting and filtering on all the available fields. This process eliminates a large portion of the work typically pushed back to the clinical manager. Their role now is focused on verifying the mappings. These relationships are saved and applied against future PO detail so that it is kept up to date.
Tying It All Together
Once costs are associated to the platforms, we need to spread those costs to the tests performed on each platform. The default approach is to spread with equal weighting to all tests, but this may not be appropriate for all spend types. For example, the main platform in Chemistry is a large, automated analyzer. Labor costs are relatively independent of volume, so equal weighting to the tests might be appropriate. Consumable supply costs (reagent kits, controls, calibrators) are not equally weighted because many billed tests are panels comprised of several individual tests, so a weighting needs to be applied. We're working on an enhanced version associating the PO line item to the exact billable test using the item, thereby creating the weight.
The resulting information is essentially a pure cost per test before being burdened with other general costs allocated within the cost center. Lab managers can use this as their marginal cost to guide pricing decisions as they seek out new business. For example, if consumable supplies are the only variable cost on a platform, new volume can be priced to cover these costs. This may allow the hospital to be competitive in acquiring non-patient business. Here is an example of a cost profile of a single test:

Summary
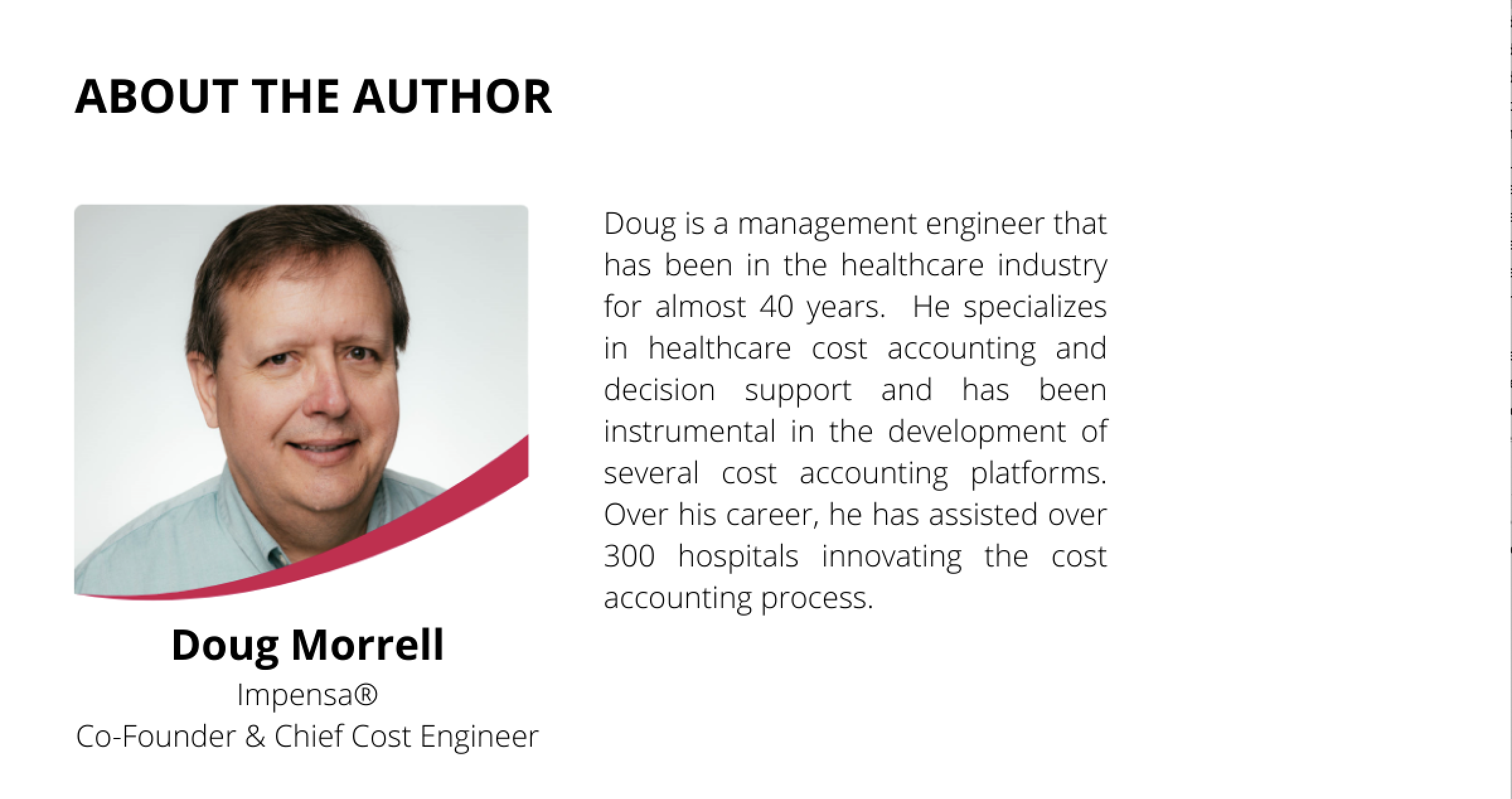
The Clinical Laboratory consumes a significant portion of hospital costs, and typically sells services outside the hospital walls. CVR projects will want to quantify potential benefits of reduced testing. Lab managers have a keen interest in the business aspects of test production. As we move into enhanced costing environments, always keep in mind that each cost center has its own requirements and methodologies to determine costs. TDABC does not apply to every situation. Leverage available data sources to rely less on estimates. And, above all, work to eliminate RCC from all costing calculations.